Introduction
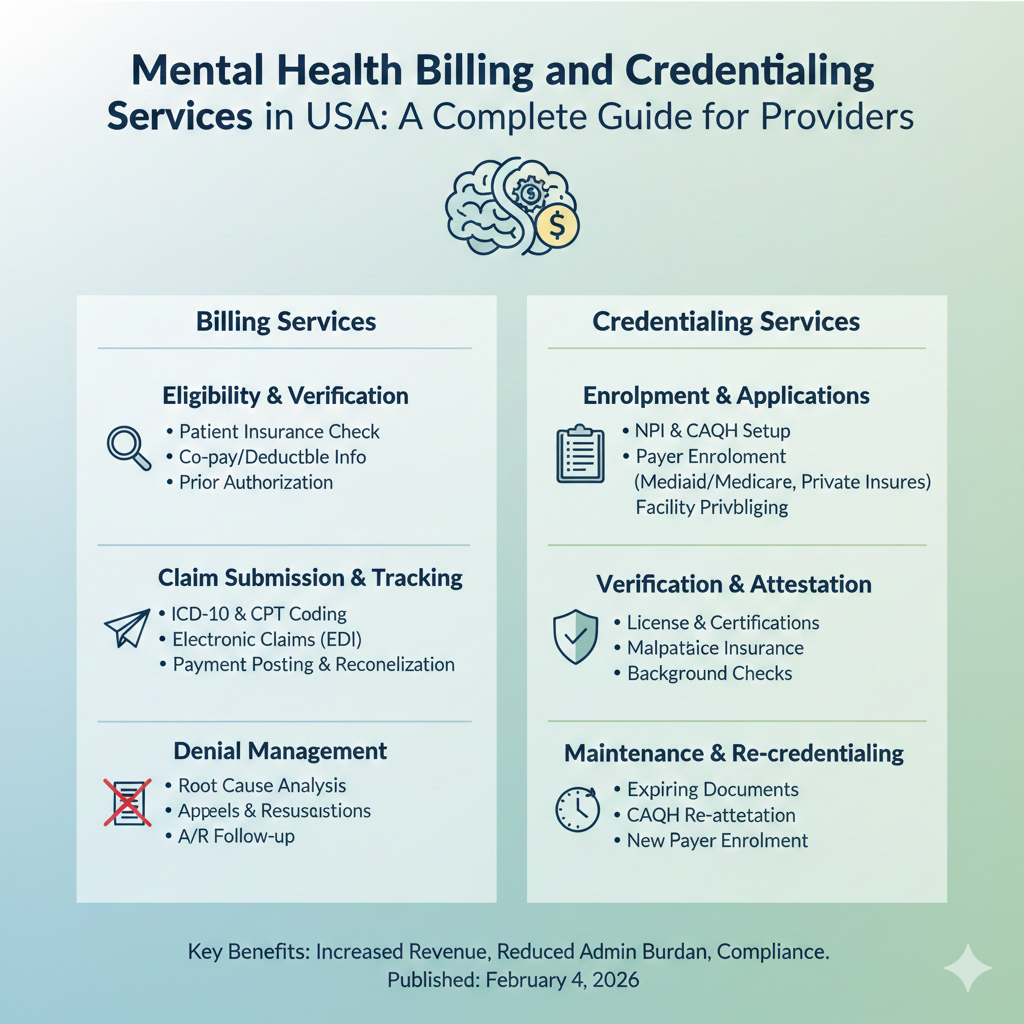
Mental health practices across the United States face growing administrative pressure as payer rules, credentialing requirements, and reimbursement standards continue to evolve. Providers want to focus on patient care, yet billing errors, delayed credentialing, and denied claims often disrupt cash flow and operations. This is where mental health billing and credentialing services play a vital role in helping practices remain compliant, efficient, and financially stable.
Whether you are a solo therapist, a group practice, or a behavioral health organization, understanding how professional billing and credentialing support works can make a measurable difference in revenue performance and long-term growth.
Why Mental Health Billing and Credentialing Matter
Mental health billing is uniquely complex compared to other medical specialties. Services often involve time-based coding, frequent policy updates, and varying documentation standards across insurers. Credentialing adds another layer of complexity, requiring accurate enrollment with payers before claims can even be submitted.
Professional billing and credentialing services help providers by:
-
Reducing claim denials and underpayments
-
Ensuring timely payer enrollment and revalidation
-
Maintaining compliance with state and federal regulations
-
Improving revenue cycle transparency
-
Allowing clinicians to spend more time with patients
Without structured support, even experienced practices can struggle to keep up with payer changes and administrative demands.
Understanding Mental Health Billing Services Across the USA
Mental health billing needs differ by state due to Medicaid programs, payer policies, and regulatory requirements. Many providers look for specialized regional expertise to ensure accuracy and faster reimbursements.
In Florida, providers frequently rely on billing services for mental health providers florida to manage high patient volumes and diverse insurance plans. A dedicated mental health billing agency florida understands state Medicaid rules, commercial payer nuances, and documentation standards required for behavioral health claims. Many practices also turn to florida mental health medical billing outsourcing services to reduce overhead and improve operational efficiency.
California presents its own challenges due to strict compliance regulations and complex payer networks. Practices often work with mental health billing companies in california or a mental health billing company california that understands Medi-Cal, commercial payers, and telehealth billing requirements. Comprehensive mental health billing services california and billing services for mental health providers california help practices navigate audits and maintain consistent reimbursements. Many providers prefer a full-service mental health billing service in california to manage everything from charge entry to denial resolution.
New York providers face dense payer networks and rigorous credentialing timelines. Mental health billing services new york and mental health billing services in new york are essential for keeping claims compliant and payments timely. Practices seeking reliability often partner with the best mental health billing company new york to manage complex authorization requirements and payer follow-ups.
In Texas, cost-efficiency is often a priority for growing practices. Many clinics search for a top mental health billing company texas or a cheap mental health billing company texas that still delivers accuracy and compliance. Similarly, practices in the Southeast and Midwest explore options such as a cheap mental health billing company north carolina or specialized mental health billing cincinnati ohio services to meet local payer demands.
The Role of Credentialing in Mental Health Practices
Credentialing is not a one-time process. It requires continuous monitoring, timely re-credentialing, and accurate documentation. Delays in credentialing can lead to months of lost revenue, especially for new providers joining a practice.
Professional mental health billing and credentialing services ensure:
-
Accurate provider enrollment with commercial and government payers
-
Timely revalidation and updates to provider information
-
Faster payer approvals for new clinicians
-
Reduced risk of claim rejections due to credentialing issues
When credentialing and billing are handled together, practices experience fewer disruptions in cash flow and smoother onboarding of new providers.
Benefits of Outsourcing Mental Health Billing and Coding
Many practices choose outsourcing mental health billing and coding services to gain access to experienced specialists without the cost of in-house staff. Outsourcing allows practices to scale efficiently while maintaining compliance and accuracy.
Key advantages include:
-
Access to certified billing and coding professionals
-
Up-to-date knowledge of payer rule changes
-
Advanced claim tracking and reporting tools
-
Reduced administrative workload for clinical staff
-
Predictable revenue cycle performance
Outsourcing also provides flexibility for practices expanding into multiple states, such as those offering mental health billing services company florida while also managing mental health billing services in california or New York.
https://www.247medicalbillingservices.com/mental-health-billing-services-new-york
Choosing the Right Billing Partner
Selecting the right billing partner is critical for long-term success. Providers should look beyond pricing and focus on experience, transparency, and communication.
Important factors to consider include:
-
Proven expertise in mental health and behavioral health billing
-
State-specific knowledge and payer relationships
-
Clear reporting and performance metrics
-
Strong credentialing support
-
Commitment to compliance and data security
A trusted partner like 247 medical billing services offers comprehensive solutions tailored to mental health providers, helping practices maintain financial stability while adapting to industry changes.
How Professional Billing Services Support Practice Growth
Effective billing and credentialing services do more than process claims. They provide insights into revenue trends, identify opportunities for optimization, and support strategic growth. Practices using professional mental health billing services california or New York often see improved collection rates and reduced days in accounts receivable.
With reliable billing support, providers can confidently expand services, hire additional clinicians, and explore telehealth options without administrative bottlenecks.
Conclusion
Mental health practices across the USA operate in a demanding regulatory and reimbursement environment. Partnering with professional mental health billing and credentialing services helps providers reduce administrative stress, improve cash flow, and maintain compliance. From Florida and California to Texas, New York, and beyond, specialized billing support enables practices to focus on what truly matters: delivering quality mental health care.
By choosing an experienced partner like 247 medical billing services, mental health providers can build a sustainable, efficient, and growth-ready practice.
FAQs
What makes mental health billing different from other medical billing services?
Mental health billing involves time-based coding, frequent policy updates, and specialized documentation requirements, making it more complex than many other specialties.
Why is credentialing important for mental health providers?
Credentialing ensures providers are properly enrolled with payers, allowing claims to be paid without delays or denials.
Can billing services handle multi-state practices?
Yes, experienced billing companies support providers operating across multiple states, including California, Florida, Texas, and New York.
Is outsourcing mental health billing cost-effective?
Outsourcing reduces staffing costs, improves accuracy, and often results in higher reimbursement rates over time.
How does 247 medical billing services support mental health practices?
They provide end-to-end billing, coding, and credentialing solutions designed specifically for mental health providers across the USA.