Introduction
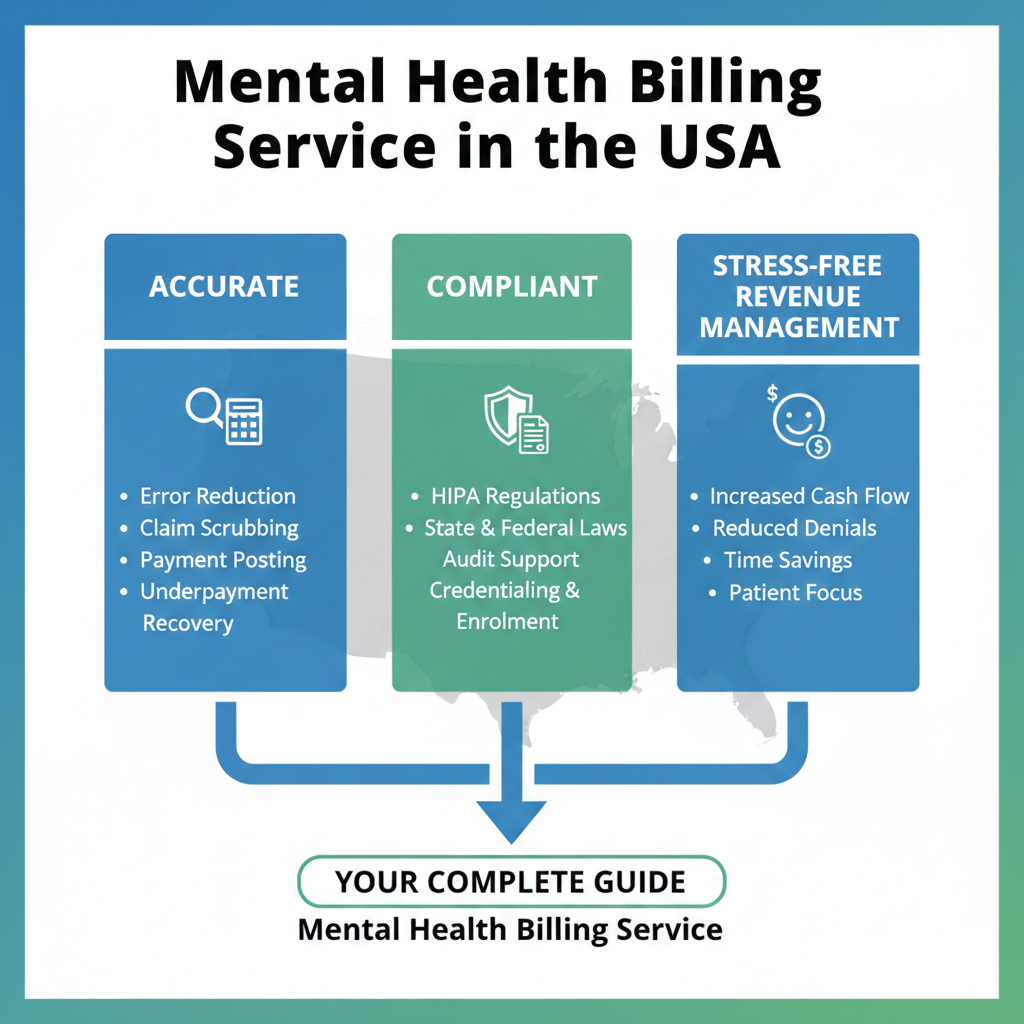
Mental health providers across the United States face a unique set of billing challenges. Unlike many other medical specialties, behavioral and mental health services involve complex coding rules, frequent authorization requirements, strict documentation standards, and ever-changing payer policies. Even small billing errors can lead to delayed payments, denials, or compliance risks.
A reliable mental health billing service plays a critical role in helping practices maintain financial stability while allowing clinicians to focus on patient care. This guide explains how mental health billing works, why it is different, and how outsourcing billing can improve accuracy, cash flow, and long-term growth for mental health practices in the USA.
What Is a Mental Health Billing Service?
A mental health billing service manages the entire revenue cycle for behavioral health providers. This includes insurance verification, coding, claim submission, payment posting, denial management, and patient billing. These services are tailored specifically for psychiatry, psychology, counseling, and therapy practices.
Mental health billing requires a deep understanding of behavioral health CPT codes, ICD-10 diagnoses, time-based services, telehealth rules, and payer-specific policies. A specialized billing service ensures that claims are submitted correctly the first time, reducing rework and revenue loss.
Why Mental Health Billing Is More Complex Than General Medical Billing
Mental health billing is governed by strict regulations and documentation standards. Many services are time-based, which means accuracy in session length, modifiers, and place of service is essential. Insurance companies also apply medical necessity criteria more aggressively to behavioral health claims.
Common complexities include:
-
Frequent prior authorization requirements
-
Session limits imposed by payers
-
Telehealth parity laws that vary by state
-
Coordination with managed behavioral health organizations
-
Increased audit risk for documentation errors
Without expert billing support, practices often struggle with high denial rates and delayed reimbursements.
Key Services Included in Mental Health Billing
A comprehensive mental health billing service typically includes:
Insurance Eligibility and Benefits Verification
Before appointments, patient coverage is verified to confirm active benefits, copays, deductibles, and session limits. This prevents unexpected denials and improves patient transparency.
Accurate Coding and Charge Entry
Correct use of CPT codes, modifiers, and diagnosis codes is critical. Mental health billing specialists stay updated on coding changes and payer-specific rules.
Claims Submission and Tracking
Claims are submitted electronically and closely monitored to ensure timely processing. Any rejections are corrected and resubmitted promptly.
Payment Posting and Reconciliation
Insurance payments and patient payments are accurately posted, allowing practices to track revenue and outstanding balances clearly.
Denial Management and Appeals
Denied claims are analyzed to identify root causes. Appeals are prepared with proper documentation to recover lost revenue.
Patient Billing and Statements
Clear, compliant patient statements improve collections while maintaining a respectful patient experience.
Benefits of Outsourcing Mental Health Billing Services
Outsourcing billing offers both financial and operational advantages for mental health practices.
Improved Cash Flow
Faster claim submission and proactive follow-ups reduce payment delays and stabilize monthly revenue.
Reduced Administrative Burden
Clinicians and staff spend less time on billing issues and more time on patient care.
Higher First-Pass Acceptance Rates
Experienced billing teams submit cleaner claims, reducing rejections and resubmissions.
Enhanced Compliance
Billing experts stay current with HIPAA, payer policies, and federal regulations, minimizing audit risks.
Scalable Support
As practices grow, billing services can easily scale without the need to hire and train in-house staff.
Mental Health Billing and Telehealth in the USA
Telehealth has become a core part of mental health care. However, billing for virtual services requires strict adherence to payer rules regarding modifiers, place of service codes, and documentation.
A specialized mental health billing service ensures that telehealth claims are submitted correctly based on federal and state regulations. This is especially important as telehealth policies continue to evolve across the USA.
Choosing the Right Mental Health Billing Partner
Selecting the right billing partner is a strategic decision. Practices should look for a company with proven experience in behavioral health billing and a strong understanding of U.S. insurance systems.
Key factors to consider include:
-
Experience with mental health and behavioral health practices
-
Transparent reporting and regular performance updates
-
Strong denial management processes
-
Knowledge of Medicare, Medicaid, and commercial payers
-
Commitment to data security and HIPAA compliance
247 Medical Billing Services works closely with mental health providers to deliver accurate, compliant, and efficient billing solutions designed to support sustainable practice growth.
Common Billing Mistakes Mental Health Practices Should Avoid
Even experienced practices can face revenue loss due to avoidable errors. Common mistakes include:
-
Using incorrect or outdated CPT codes
-
Missing documentation for medical necessity
-
Billing incorrect session lengths
-
Failing to verify insurance benefits in advance
-
Delayed follow-up on denied claims
A professional billing service helps eliminate these issues through structured workflows and ongoing quality checks.
How Mental Health Billing Services Support Practice Growth
Beyond claim submission, a strong billing partner provides insights into practice performance. Detailed reports on revenue trends, denial patterns, and payer behavior help practices make informed business decisions.
With consistent cash flow and fewer administrative distractions, mental health providers can expand services, hire additional clinicians, and invest in better patient care.
Conclusion
Mental health providers play a vital role in supporting emotional and psychological well-being, but billing challenges can undermine even the most dedicated practices. A specialized mental health billing service ensures accurate coding, timely reimbursements, and regulatory compliance while reducing administrative stress.
By partnering with an experienced provider like 247 Medical Billing Services, mental health practices in the USA can protect their revenue, improve operational efficiency, and focus fully on what matters most—patient care.
Frequently Asked Questions
What types of providers benefit from mental health billing services?
Psychiatrists, psychologists, therapists, counselors, and behavioral health clinics all benefit from specialized billing support.
Is mental health billing different for Medicare and Medicaid?
Yes. Medicare and Medicaid have distinct coverage rules, documentation requirements, and reimbursement structures that require expert handling.
Can a billing service help with denied claims?
A professional billing service actively manages denials, prepares appeals, and works to recover lost revenue.
How does outsourcing billing affect patient experience?
When done correctly, outsourcing improves accuracy and transparency, resulting in clearer statements and fewer billing disputes.
Is mental health billing service suitable for small practices?
Yes. Small and solo practices often benefit the most, as outsourcing reduces overhead and ensures consistent revenue without hiring in-house staff.