Antibiotic resistance in Nigeria has rapidly grown into a critical public health issue, threatening the ability to treat common infections and undermining decades of medical progress. Once-curable diseases are now becoming difficult—or even impossible—to treat due to the overuse and misuse of antibiotics. The growing prevalence of drug-resistant bacteria across hospitals and communities has raised serious concerns among health professionals, policymakers, and global health organizations. In this article, we explore the causes, impacts, and urgent solutions to combat antibiotic resistance in Nigeria, while emphasizing the need for a collective national response.
What Is Driving Antibiotic Resistance in Nigeria?
Unregulated Access and Misuse of Antibiotics
One of the biggest drivers of antibiotic resistance in Nigeria is the widespread and unregulated access to antibiotics. In many areas, people can walk into local pharmacies or patent medicine stores and buy antibiotics without a prescription. This has led to rampant misuse—such as self-medicating for viral infections, using the wrong drugs, or not completing the full course of treatment.
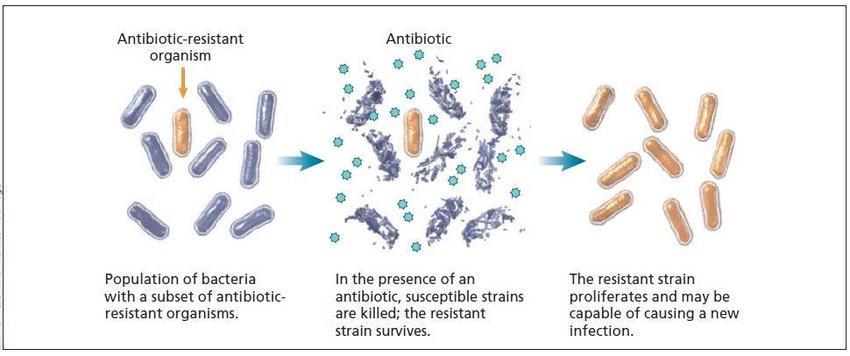
This misuse increases the chances that bacteria will evolve to resist these medications. The more antibiotics are used incorrectly, the more bacteria adapt, rendering these drugs ineffective over time.
Weak Diagnostic and Laboratory Infrastructure
In many Nigerian healthcare facilities, doctors and health workers prescribe antibiotics without proper diagnostic tests. This is not by choice but due to a lack of functioning diagnostic laboratories or resources to conduct tests. Without the ability to confirm what type of bacteria is causing an infection, many practitioners rely on guesswork, leading to overprescription or inappropriate drug choices.
This empirical treatment approach contributes significantly to antibiotic resistance in Nigeria, as it encourages the survival and spread of resistant bacterial strains.
Low Awareness Among the Public and Healthcare Workers
Public knowledge about antibiotic resistance remains dangerously low. Many Nigerians still believe antibiotics can treat all kinds of infections, including viral illnesses like the flu or common cold. Additionally, some patients pressure healthcare providers into prescribing antibiotics even when they are not necessary.
Surprisingly, the knowledge gap also exists among healthcare professionals. Medical and pharmacy students, nurses, and even some doctors lack comprehensive training on antimicrobial stewardship and the responsible use of antibiotics. This contributes to incorrect prescribing practices and further fuels resistance.
Economic Challenges and Counterfeit Drugs
The rising cost of antibiotics, inflation, and lack of local production have made high-quality antibiotics less affordable and accessible for many Nigerians. As a result, patients often buy incomplete doses or resort to cheaper alternatives, which are sometimes counterfeit or substandard.
Counterfeit medications not only fail to treat infections but also allow bacteria to build resistance. The economic burden of antibiotic resistance in Nigeria is profound—not just in medical costs but also in lost productivity and increased mortality.
The Impact on Healthcare Outcomes
Antibiotic resistance in Nigeria is already having severe consequences for healthcare delivery and patient outcomes. Hospitals are seeing a rise in difficult-to-treat infections, longer hospital stays, and increased mortality—especially among vulnerable populations such as newborns, the elderly, and people with weakened immune systems.
Drug-resistant infections cost more to treat, often requiring stronger, second-line antibiotics that are more expensive and have more side effects. In some cases, no effective treatment is available at all.
This growing resistance crisis has also put a strain on hospital resources, with more time, medication, and care required for each patient. Moreover, the fear of untreatable infections may discourage people from seeking timely medical care, further complicating the public health response.
How Nigeria Can Respond: Practical Solutions
Tackling antibiotic resistance in Nigeria requires a multi-pronged approach that involves the government, healthcare sector, civil society, and the general public. Here are some critical steps:
1. Strengthen Regulation of Antibiotics
There needs to be stricter enforcement of prescription-only policies for antibiotics. Pharmacies and drug vendors must be monitored to prevent over-the-counter sales without proper medical authorization. Regulatory agencies must ensure that only safe and quality-assured antibiotics are available in the market.
2. Expand Diagnostic Capacity
To reduce blind prescribing, Nigeria must invest in diagnostic laboratories across primary and secondary healthcare centers. This will enable accurate detection of bacterial infections and ensure that antibiotics are prescribed only when necessary.
Rapid diagnostic tools can also help healthcare providers select the most effective antibiotic, reducing unnecessary use of broad-spectrum drugs that promote resistance.
3. Promote Antimicrobial Stewardship Programs
Antimicrobial stewardship programs (ASPs) are structured efforts within hospitals and clinics to optimize antibiotic use. These programs train healthcare workers on when and how to prescribe antibiotics appropriately, review patient prescriptions, and monitor antibiotic use across departments.
Nigeria must prioritize the implementation of ASPs in all healthcare facilities, especially tertiary hospitals where the burden of drug-resistant infections is highest.
4. Increase Public Awareness and Health Education
Changing public behavior is vital. National awareness campaigns should educate the public on the dangers of antibiotic misuse, the importance of completing prescribed treatments, and the role of hygiene and vaccinations in preventing infections.
Schools, religious institutions, and community centers can serve as platforms for these awareness programs. Healthcare workers should also be equipped with the tools to communicate these messages effectively.
5. Support Local Production of Quality Antibiotics
Reducing dependence on imported antibiotics will help stabilize supply and potentially lower prices. Nigeria should invest in its pharmaceutical manufacturing sector to produce high-quality, affordable antibiotics locally. This can also reduce the risk of counterfeit medications flooding the market.
6. Improve Infection Prevention and Control
Basic measures such as hand hygiene, sanitation, clean water, and waste management can reduce the spread of infections and lessen the need for antibiotics in the first place. Healthcare facilities must adopt strict infection prevention and control protocols, including sterilization of equipment and isolation of patients with drug-resistant infections.
Conclusion
Antibiotic resistance in Nigeria is a silent but rapidly escalating crisis. It threatens not only the health of individuals but also the stability of the country’s healthcare system. If left unchecked, it could lead to a future where minor infections become deadly once again.
However, this outcome is not inevitable. By taking urgent action—strengthening regulation, investing in diagnostics and local drug production, improving public awareness, and promoting responsible antibiotic use—Nigeria can reverse the trend and protect future generations.
Combating antibiotic resistance in Nigeria will require collective effort and political will, but the payoff is clear: healthier communities, stronger healthcare systems, and a safer, more resilient nation.